My Personal Experience, Diagnosis, and Treatments
Summary: After going to the doctor with back pain in 1981, I was diagnosed with Scheuermann’s Kyphosis/Disease at the age of 17. I wore a Milwaukee brace for a year at the age of 20 in hopes of straightening my curvature and strengthening my core muscles.
The disease has caused progressively acute back, arm, and leg pain while limiting my activities and movement. I kept to doctor’s orders by keeping my weight down and staying in good shape and was able to stave off surgery until 2007.
At this point, I was almost unable to walk as pain significantly increased and daily activities became all but impossible. Since then, I have had 6 serious spinal surgeries in an effort maintain the use of my limbs due to lack of blood supply to the nerves controlling their movement.
The following information offers a glimpse into my past and the challenges faced.
Bottom line: Since I was diagnosed late in life (after adolescence), prognosis and outcome of is not as positive as it would have been had the diagnosis been made before adolescence.
The disease has caused progressively acute back, arm, and leg pain while limiting my activities and movement. I kept to doctor’s orders by keeping my weight down and staying in good shape and was able to stave off surgery until 2007.
At this point, I was almost unable to walk as pain significantly increased and daily activities became all but impossible. Since then, I have had 6 serious spinal surgeries in an effort maintain the use of my limbs due to lack of blood supply to the nerves controlling their movement.
The following information offers a glimpse into my past and the challenges faced.
Bottom line: Since I was diagnosed late in life (after adolescence), prognosis and outcome of is not as positive as it would have been had the diagnosis been made before adolescence.
My Personal Experience
The reason for giving my background and history is not to offer everyone a detailed account of my life (much too boring to put in print), but rather, to help people understand the hurdles that people face with Scheuermann’s Kyphosis/Disease. It is so important for afflicted individuals to know that they are not alone in their fight against this disease. And as a note, I hold no affiliation, designation, or legal certification that qualifies me for any type of physical or mental therapy. So relax, this is more of a self-therapy exercise than anything else.…..
Many of my thoughts and feelings are written in hindsight, which we all know is 20-20. At the time of my diagnosis, information, physical therapy, treatment options, device and mechanical assistance, and long-term prognosis was extremely limited. It would be easy for all of us to judge the decisions of diagnosticians explained in this information. However, the recommendations were made in my best interest and with all the pertinent and relevant information available at the time. Remember, this has been 20 years in the making.
“Pittsburgh entered the core of my heart when I was a boy and cannot be torn out.”
Andrew Carnegie
I was born (1964) and raised in Pittsburgh, PA (Go Steelers and Penguins!! Need a new owner for the Pirates, though), always energetic and active as a child. Pittsburgh has always been a tough, sports-minded city. Following true to form, my friends and I would ride our bikes in the morning, go home to eat lunch, play kill-the-man-with-the-ball in the afternoon, eat dinner, and finally play kick-the-can or it-tag in the evening. Man, it would be great to have that energy again……
Pittsburgh schools typically had 3 seasons of sports for Boys: fall (football), winter (basketball, wrestling), and spring (track, baseball). My personal favorites were football and basketball.
My youth football career was very limited since my Mom wouldn’t allow me play Pee-Wee football (she was afraid of one of my bone growth plates breaking) so I started playing in 7th grade. This is when I first noticed back pain. Anytime that I made a tackle there was this intense pain in my lower back. We didn’t have the best (or any) medical trainers at the time so the coach had me wear a foam pad taped to my lower back for practices and games. Not sure what caused me to remember this, but as I look back, my body was giving me some warning signs about limiting activities. I played little football in high school after I figured out that basketball was more my sport.
I started playing basketball in 6th grade at the age of 12 in the YBA. We had a great coach who had a basketball mind and taught us basketball’s true fundamentals. Coach really got me interested in the sport and I played through high school with some success. Playing basketball over time made me realize that something was wrong with my back as the pain was beginning to get pretty bad. The pain was site specific, between my shoulder blades and in my lower back. My neck also required “cracking” all the time. I would bend my neck to either side and my neck would “pop” like a zipper. Guess I wasn’t the brightest bulb in the bunch now that I look back…..
Many of my thoughts and feelings are written in hindsight, which we all know is 20-20. At the time of my diagnosis, information, physical therapy, treatment options, device and mechanical assistance, and long-term prognosis was extremely limited. It would be easy for all of us to judge the decisions of diagnosticians explained in this information. However, the recommendations were made in my best interest and with all the pertinent and relevant information available at the time. Remember, this has been 20 years in the making.
“Pittsburgh entered the core of my heart when I was a boy and cannot be torn out.”
Andrew Carnegie
I was born (1964) and raised in Pittsburgh, PA (Go Steelers and Penguins!! Need a new owner for the Pirates, though), always energetic and active as a child. Pittsburgh has always been a tough, sports-minded city. Following true to form, my friends and I would ride our bikes in the morning, go home to eat lunch, play kill-the-man-with-the-ball in the afternoon, eat dinner, and finally play kick-the-can or it-tag in the evening. Man, it would be great to have that energy again……
Pittsburgh schools typically had 3 seasons of sports for Boys: fall (football), winter (basketball, wrestling), and spring (track, baseball). My personal favorites were football and basketball.
My youth football career was very limited since my Mom wouldn’t allow me play Pee-Wee football (she was afraid of one of my bone growth plates breaking) so I started playing in 7th grade. This is when I first noticed back pain. Anytime that I made a tackle there was this intense pain in my lower back. We didn’t have the best (or any) medical trainers at the time so the coach had me wear a foam pad taped to my lower back for practices and games. Not sure what caused me to remember this, but as I look back, my body was giving me some warning signs about limiting activities. I played little football in high school after I figured out that basketball was more my sport.
I started playing basketball in 6th grade at the age of 12 in the YBA. We had a great coach who had a basketball mind and taught us basketball’s true fundamentals. Coach really got me interested in the sport and I played through high school with some success. Playing basketball over time made me realize that something was wrong with my back as the pain was beginning to get pretty bad. The pain was site specific, between my shoulder blades and in my lower back. My neck also required “cracking” all the time. I would bend my neck to either side and my neck would “pop” like a zipper. Guess I wasn’t the brightest bulb in the bunch now that I look back…..
My Diagnosis
The doctor’s diagnosis of my SD was made in 1981 when I was 17 years old. It was spring and I was trying out for the high school track team in the javelin. If you have ever seen anyone throw the javelin, you will notice that you are required to arch your back so that your body acts as a spring to jettison the javelin. Well, I had difficulty with the back arch and went to see my family physician (so fortunate to have such a wonderful family physician growing up), who, in turn, sent me to a specialist.
Fortunately, I was blessed to have a tremendous Orthopedic Surgeon who properly diagnosed my SK immediately. I was started on a regimen of anti-inflammatory drugs and given an exercise schedule, which included:
It took me a while to listen to the doctor when it pertained to exercise, since I was so young and stupid. We all feel invincible at that age, but wish I would have listened.
After a couple years of significantly strengthening my body, my orthopedic surgeon recommended that I wear a Milwaukee brace for a year. This white plastic brace would stretch from my neck to my hips and needed to be worn during waking hours. So, at the age of 20, I was fitted for, and wore, the Milwaukee brace for a year (it is still sitting in my parents’ attic). That was lots o’ fun, considering that I was a summer camp counselor and attended college during this time. However, I did wear the brace as prescribed and followed the doctor’s orders.
“Three rules: I do not eat too much; I do not worry too much; and, if I do my best, I believe that what happens, happens for the best.”
Henry Ford
My parents have always instilled in their children that no matter what you do, do it with grace, dignity, and work your hardest. So, I graduated from college with 2 degrees, Business/Finance and International Studies in 4 years and started work as a stockbroker three days after commencements. I initially wanted to help people medically, but freshman biology took care of that aspiration. So, if I couldn’t help people medically, I figured that I could help them financially, and that is what I have done my entire life.
It was pretty evident early-on that I needed a passion in work to be successful, and the opportunity to help people financially has always provided that spark. It has been so comforting to know that so many people have been helped over the years and it makes my life’s work much more meaningful, which is very important to me.
As life would have it, the business environment in the financial services industry has been, to put it mildly, rather tumultuous. The nature of the business has required a number of relocations (13 to be exact) to different cities, due to promotions, transfers, and new jobs. My occupation has also required extensive travel, via both car and plane.
I realize that these moves have always been my choice, so I am not complaining in the least. My life has exceeded all my youthful expectations and I wouldn’t trade any of these experiences for anything. There are two wall maps in my office, one of the United States and one of the world, with pins that denote all the places that I have visited. Sometimes I look at the maps in amazement and wonder how cool life has been. I have truly been blessed.
“Life is what happens to you while you're busy making other plans”
John Lennon
During this time I continued to exercise and keep my weight down. Being 6’3” and 245 pounds, nobody would have guessed that I was in pain. I always prided myself on being in relatively good shape, but did notice increased pain all over my body. It seemed to radiate down my arms and legs and simple tasks became more difficult. The work travel was really taking a toll. Whether it was driving or flying, the pain was not subsiding.
Our family has a rather stoic demeanor when it comes to pain. We would rather work through the difficult times and keep positive attitudes than share our discomfort with others. Right or wrong, that is just how we are.
We do, however, have one outstanding quirk: sweating. Oh yes, very attractive indeed. So as I drove and flew all over the country for work, I was a perpetual sweating machine. Too bad we can’t harness it into a power source because we would be really wealthy family.
My point in discussing the pain associated with frequent traveling is that individuals afflicted with uncorrected or untreated SK may want to take this into consideration when choosing a career. Just a thought.
“Don't let what you cannot do interfere with what you can do."
John Wooden
During this time in my life, my exercise routines became more and more limited. Contact sports were the first to go. The annual turkey-bowl pickup football game fell by the wayside after college. No more participation in pickup basketball leagues, this ended in 1991. The pain in my back, legs, and arms lasted for days after games and rigorous running or pounding activities.
So with group sports out of the question, I searched for individual sports that would allow me to work off stress and keep me in shape. I tried golf, but twisting while swinging a club was as agonizing as my score. Tennis and racquetball were out because of the same twisting problem. Swimming was almost impossible due to the inability to arch my back to breathe, unless I grew gills. My brother and I started mountain biking, which was a blast. Unfortunately, I had a hard time with the pounding of the trails so had to stop (my brother continues his mountain biking to this day).
Finally, my brother-in-law recommended lifting weights, so I worked out an exercise regimen with my doctors. This really sparked an interest for me. Over time, the added muscle seemed to help keep my spine strong and delay the onset of more serious symptoms. My doctors advised me to stay away from squats and deadlifts, plus to limit the amount of weight lifted over my head (military presses) and I kept to these recommendations pretty firmly.
The added muscle did seem to keep my pain level constant for a while but it was important to listen to my body. As exercises caused more pain (not the workout hurt, but the bad kind of hurt) I decreased the weight or cut out these exercises all together.
For years I was able to keep a somewhat consistent workout schedule of 2-4 times a week (which also included the use of an elliptical machine), even with the extensive traveling. It was important for me to maintain my weight by exercising and think I would have gone nuts had there been no way to reduce the stress level associated with constant pain. Sitting in a car for hours or on an airport tarmac is not a pleasant experience when the pain is so bad that you sweat through your suits. Yes, a nice vision.
Massage therapy, by a licensed therapist, was also an excellent tool for dealing with the back and leg/arm pain. After trying a number of different techniques, deep tissue massage worked the best for me. I would often go 2 times a week for the deep tissue work and this seemed to relieve some of the stress and pain throughout my body. I kept up with the massage therapy for a few years, at least until the nerves were too sensitive for me to continue on a regular basis.
Many of my friends also recommended acupuncture, so I gave that a shot, too. Unfortunately, after several treatments, my pain did not decrease.
Another thing that I noticed was that my sleep patterns suffered significantly. The constant pain kept me from getting much sleep and I was up and down all night. One night I finally reached my breaking point and had a seizure for about 4 hours. After working with 9 different doctors in various specialties it was determined that my pain was keeping me from reaching the deep sleep necessary for my body to heal. In fact, after I completed a sleep study, I was diagnosed with zero deep sleep. This was a huge issue since my work kept me on a fast pace and sleep was extremely important for my recovery from the stress.
To give you an idea how this feels, imagine the worst jet lag you have ever felt; then feel that way for years. Even though you may sleep (and even snore!), you never feel rested.
Fortunately, I have worked with a number of excellent doctors over the last 20 years who have helped to develop various prescription drug combinations for me to use as sleep aids. Even with these prescriptions (with adjustments of content and quantity over time), quality rest continues to be elusive. I am able to sleep but my body still does not attain the proper level of necessary deep sleep. Ugh….all these prescriptions and I never even took an aspirin when I was young.
Another issue that arose as a result of the pain and sleep deprivation was the constant grinding of my teeth at night (I lost count at 17 broken teeth and fillings). In order for me to lessen the damage to my teeth and jaws, I was required to wear a hard mouth night guard, or “bit” as I like to call it, while sleeping. I consistently bite through and break these night guards, but I still have my teeth!!
Fortunately, I was blessed to have a tremendous Orthopedic Surgeon who properly diagnosed my SK immediately. I was started on a regimen of anti-inflammatory drugs and given an exercise schedule, which included:
- Not getting fat! I would always have to keep the fat off my body as it would cause too much stress on my lower back if I had too large of a stomach.
- Doing at least 100-200 sit-ups a day, with nothing holding my legs.
- Limit the weight and exercises that required me to reach above my head.
- Stay away from pounding sports such as football, basketball, and racquet sports.
It took me a while to listen to the doctor when it pertained to exercise, since I was so young and stupid. We all feel invincible at that age, but wish I would have listened.
After a couple years of significantly strengthening my body, my orthopedic surgeon recommended that I wear a Milwaukee brace for a year. This white plastic brace would stretch from my neck to my hips and needed to be worn during waking hours. So, at the age of 20, I was fitted for, and wore, the Milwaukee brace for a year (it is still sitting in my parents’ attic). That was lots o’ fun, considering that I was a summer camp counselor and attended college during this time. However, I did wear the brace as prescribed and followed the doctor’s orders.
“Three rules: I do not eat too much; I do not worry too much; and, if I do my best, I believe that what happens, happens for the best.”
Henry Ford
My parents have always instilled in their children that no matter what you do, do it with grace, dignity, and work your hardest. So, I graduated from college with 2 degrees, Business/Finance and International Studies in 4 years and started work as a stockbroker three days after commencements. I initially wanted to help people medically, but freshman biology took care of that aspiration. So, if I couldn’t help people medically, I figured that I could help them financially, and that is what I have done my entire life.
It was pretty evident early-on that I needed a passion in work to be successful, and the opportunity to help people financially has always provided that spark. It has been so comforting to know that so many people have been helped over the years and it makes my life’s work much more meaningful, which is very important to me.
As life would have it, the business environment in the financial services industry has been, to put it mildly, rather tumultuous. The nature of the business has required a number of relocations (13 to be exact) to different cities, due to promotions, transfers, and new jobs. My occupation has also required extensive travel, via both car and plane.
I realize that these moves have always been my choice, so I am not complaining in the least. My life has exceeded all my youthful expectations and I wouldn’t trade any of these experiences for anything. There are two wall maps in my office, one of the United States and one of the world, with pins that denote all the places that I have visited. Sometimes I look at the maps in amazement and wonder how cool life has been. I have truly been blessed.
“Life is what happens to you while you're busy making other plans”
John Lennon
During this time I continued to exercise and keep my weight down. Being 6’3” and 245 pounds, nobody would have guessed that I was in pain. I always prided myself on being in relatively good shape, but did notice increased pain all over my body. It seemed to radiate down my arms and legs and simple tasks became more difficult. The work travel was really taking a toll. Whether it was driving or flying, the pain was not subsiding.
Our family has a rather stoic demeanor when it comes to pain. We would rather work through the difficult times and keep positive attitudes than share our discomfort with others. Right or wrong, that is just how we are.
We do, however, have one outstanding quirk: sweating. Oh yes, very attractive indeed. So as I drove and flew all over the country for work, I was a perpetual sweating machine. Too bad we can’t harness it into a power source because we would be really wealthy family.
My point in discussing the pain associated with frequent traveling is that individuals afflicted with uncorrected or untreated SK may want to take this into consideration when choosing a career. Just a thought.
“Don't let what you cannot do interfere with what you can do."
John Wooden
During this time in my life, my exercise routines became more and more limited. Contact sports were the first to go. The annual turkey-bowl pickup football game fell by the wayside after college. No more participation in pickup basketball leagues, this ended in 1991. The pain in my back, legs, and arms lasted for days after games and rigorous running or pounding activities.
So with group sports out of the question, I searched for individual sports that would allow me to work off stress and keep me in shape. I tried golf, but twisting while swinging a club was as agonizing as my score. Tennis and racquetball were out because of the same twisting problem. Swimming was almost impossible due to the inability to arch my back to breathe, unless I grew gills. My brother and I started mountain biking, which was a blast. Unfortunately, I had a hard time with the pounding of the trails so had to stop (my brother continues his mountain biking to this day).
Finally, my brother-in-law recommended lifting weights, so I worked out an exercise regimen with my doctors. This really sparked an interest for me. Over time, the added muscle seemed to help keep my spine strong and delay the onset of more serious symptoms. My doctors advised me to stay away from squats and deadlifts, plus to limit the amount of weight lifted over my head (military presses) and I kept to these recommendations pretty firmly.
The added muscle did seem to keep my pain level constant for a while but it was important to listen to my body. As exercises caused more pain (not the workout hurt, but the bad kind of hurt) I decreased the weight or cut out these exercises all together.
For years I was able to keep a somewhat consistent workout schedule of 2-4 times a week (which also included the use of an elliptical machine), even with the extensive traveling. It was important for me to maintain my weight by exercising and think I would have gone nuts had there been no way to reduce the stress level associated with constant pain. Sitting in a car for hours or on an airport tarmac is not a pleasant experience when the pain is so bad that you sweat through your suits. Yes, a nice vision.
Massage therapy, by a licensed therapist, was also an excellent tool for dealing with the back and leg/arm pain. After trying a number of different techniques, deep tissue massage worked the best for me. I would often go 2 times a week for the deep tissue work and this seemed to relieve some of the stress and pain throughout my body. I kept up with the massage therapy for a few years, at least until the nerves were too sensitive for me to continue on a regular basis.
Many of my friends also recommended acupuncture, so I gave that a shot, too. Unfortunately, after several treatments, my pain did not decrease.
Another thing that I noticed was that my sleep patterns suffered significantly. The constant pain kept me from getting much sleep and I was up and down all night. One night I finally reached my breaking point and had a seizure for about 4 hours. After working with 9 different doctors in various specialties it was determined that my pain was keeping me from reaching the deep sleep necessary for my body to heal. In fact, after I completed a sleep study, I was diagnosed with zero deep sleep. This was a huge issue since my work kept me on a fast pace and sleep was extremely important for my recovery from the stress.
To give you an idea how this feels, imagine the worst jet lag you have ever felt; then feel that way for years. Even though you may sleep (and even snore!), you never feel rested.
Fortunately, I have worked with a number of excellent doctors over the last 20 years who have helped to develop various prescription drug combinations for me to use as sleep aids. Even with these prescriptions (with adjustments of content and quantity over time), quality rest continues to be elusive. I am able to sleep but my body still does not attain the proper level of necessary deep sleep. Ugh….all these prescriptions and I never even took an aspirin when I was young.
Another issue that arose as a result of the pain and sleep deprivation was the constant grinding of my teeth at night (I lost count at 17 broken teeth and fillings). In order for me to lessen the damage to my teeth and jaws, I was required to wear a hard mouth night guard, or “bit” as I like to call it, while sleeping. I consistently bite through and break these night guards, but I still have my teeth!!
My Treatment
Up until 2007 I was able to delay surgeries with diet, exercise, non-invasive treatments, and a high tolerance for pain. Pain killers were never an option given my profession. You need to not only be an extremely effective communicator in the financial services industry, but you also need a clear and concise mind. I never have felt that either of these required qualities was possible if given prescription narcotics on a regular basis.
However, there have been some prescriptions that seem to work the best for me: NSAID’s (non-steroidal anti-inflammatory drugs). There are some risks in taking these drugs but they take the edge off the constant pain and make me less grumpy. However, I can’t take these after spinal fusion surgeries since the bones need the inflammation to fuse properly. This poses a problem given the number of my spinal fusions over the last 4 years (as described in the following text).
But you never plan or prepare for the day when the simplest activities cause excruciating pain. Walking, sitting, sleeping, or standing (oh man, standing stationary was, and still is, the WORST pain) became so difficult that it was almost impossible to make it through a workday. That was the catalyst for me to seek out medical professionals in neurology as well as spinal orthopedics.
I met with a number of different specialists and chose to work with an excellent neurosurgeon in Indianapolis. The doctor ordered a number of spinal tests: CT scan, x-rays, and MRI so that the extent of my degeneration could be assessed. Our first appointment was very memorable as we discussed the test results. He told me that the degeneration was extensive in my entire spine and the x-rays looked like they were from someone 30 years my elder! It wasn’t that the comment was surprising, it was just that I was expecting this happen when I was much older, not in my early 30’s.
The doctor recommended different treatments before any surgical procedure was considered. The first non-invasive treatment was the use of traction. This involved me lying on a special table on my back, (the table was similar to that in a massage therapist’s room). They strapped me onto the table with a belt affixed around my waist. Weights were placed onto a pulley system which was in turn attached to the waist belt. Progressively higher weights were added to the pulleys which then pulled on my legs to help decompress the spine. Unfortunately, I lost the feeling in my left foot after a few treatments so the doctor recommended that the traction cease.
The next step on the treatment trail was injection of cortisone into the inflamed nerves in my lumbar spine. If that sounds fun, then you are right. The shots weren’t like getting a flu vaccine in your arm. Evidently it is important to inject the inflamed nerve vveerryy sslloowwllyy with the cortisone. I will never forget the look on my doctor’s face when I turned around and looked at him with sweat on my brow and said, “You are never doing that to me again.” Thought he was going to immediately bolt out of the room.
The cortisone was intended to relieve some of the inflammation and pain in my nerve, but any relief was short-lived as the pain quickly returned within hours. My doctor and I then discussed the next level of treatment, which was to attempt to relieve the pain from the foraminal stenosis in my lower back. As the vertebral canals (containing the nerves controlling the leg movement and sensation) narrowed, pressure was being placed on the nerve roots causing pain. This was starting to significantly alter my life, from unending insomnia to limited activity and movement. At the time, I was living in Indianapolis and did not have any family living nearby. Thankfully, my wonderful family came to the rescue.
With the operation quickly approaching, my parents (both in their 70’s) made the trip from Pittsburgh to Indianapolis to help me during the surgery and recovery process. Somewhat embarrassing for a grown man in his 40’s to have his parents take care of him, but thank God they were there to help.
The goal of the surgery was to remove bone in the lumbar canal that was pressing on my nerve roots. This, in turn, would hopefully relieve the pain and improve motor function.
The day of the operation, my parents waited patiently for word from the neurosurgeon. Finally, he appeared in the waiting room and informed my parents that my nerve roots (L5) were just “smashed” from the narrowing of the spinal canal. Fortunately, the doctor was able to expand the vertebral canal and relieve some of the pressure on my nerve roots, but only time would tell if the surgery was successful.
Recovery was slow and painful. My parents stayed with me for about a week, then my awesome sister made the trek to Indianapolis to help me for another week. She showed the patience of a saint in taking care of me for that week. I was a little grumpy to say the least. My family has been so supportive, what a true blessing.
My employer was amazingly generous and understanding as I limped my way back to work after a couple of weeks. People would often find me lying down on my office floor reading because being upright was so painful.
The purpose behind explaining the treatment and therapy process is that I don’t want anyone to think that surgery was thought of lightly. I delayed this invasive procedure as long as possible. I know there are people out there living with SK and are considering surgery, so don’t feel that you are alone in the quandary. As my doctors have always told me, treatment varies by person and only you can make an informed decision that is best for you.
“I learned a long time ago that minor surgery is when they do the operation on someone else, not you.”
Bill Walton
I eventually made a partial recovery but the pain persisted and my physical activities still had to be curtailed. Not long after the surgery, my employer was bought out 2 times in 6 weeks and my position at the bank was eliminated. Our awesome team of financial services professionals quietly moved to other jobs or companies. I found myself out of work and the pain was increasing daily.
I was fortunate to find work quickly and started work with an exceptional employer in Austin, TX. This job required relocation to Austin and travel on a weekly basis (mostly flying). I figured that I could deal with the pain of being on the road again and felt fortunate to have the opportunity to work for such a successful company. So my girlfriend and I packed up the two cats and headed for Texas.
Traveling nationally for work was more of a pain than expected, literally. Sitting in a cramped space for hours on end proved to be a real challenge. The pain was mostly in my lower back and legs. A sharp, needle like pain in my lumbar region that radiated down both legs. It got so bad sometimes that I was drenched in sweat by the time the plane landed. Plus, security procedures following 9/11 (both my brother and I were on planes that terrible morning in 2001 that were forced to land) made waiting times on the tarmac longer, which increased my pain. Necessary steps given the scary world of the 21st century, but difficult to weather with the pain.
Work was going well and we were adjusting to our new lives as Texans. I continued to travel weekly and was mostly able to keep my workout routine of 3 times a week. The workouts included light weight and elliptical training which not only relieved stress but also improved my mobility.
It was after about a year of this routine when I noticed that my arms and hands became numb and tingly after workouts. The numbness got so bad that I couldn’t open the locker or car door immediately following training. I figured that given my past shoulder problems that I slept wrong and just pinched some nerves.
After a while of dealing with the arm and hand sensations, I scheduled an appointment with a rheumatologist in Austin. The medical files from my doctors in Indianapolis were forwarded to the rheumatologist and we had an initial consult. The doctor ordered some tests and we scheduled another appointment to discuss the results.
This next appointment was a turning point in my medical life as the doctor said that there was nothing that he could do to help me. He recommended that I see a neurosurgeon as there were significant problems with my entire spine. However, he said that the primary focus was to be my cervical area. This came as a shock since my neck never really gave me that many problems. Sure it was stiff most of the time, but hey, who doesn’t have a stiff neck?
I then consulted with a recommended neurosurgeon who ordered some additional tests. The results were shocking. There were little, if any, discs remaining in most of my neck. The discs were almost completely gone between C3 and C6. This was the cause of my arm and hand sensations and hopefully the nerve damage would not be permanent. The recommendation was immediate fusion of C3-C6 with the use of cadaver bones. An incision would be made through my throat with screws and plates inserted on the anterior, or inside, of my spine to hold it secure until fusion occurred. I would be in a cervical collar for about 3 months and travel would be curtailed until then.
My employer was notified and they were GREAT about it. Their major concern was for my health and they encouraged me to do what I needed to get better.
So, I went in for surgery in June of 2008 and had the C3-C6 fusion surgery. My stay in the hospital short and 2 days later I was home resting uncomfortably. After 3 weeks I was back to work at a desk job until the neurosurgeon cleared me to travel. Wearing the cervical collar 24 hours a day was a pain in the butt, but necessary.
Three months later, work travel resumed and I was back in the swing of things. Physical therapy, including deep tissue massage, was begun and progress was slow and tedious.
It was great getting back to my full work schedule, both mentally and physically. Being up and around made me feel alive again, but there was still some lingering effects of the nerve damage to my arms. The tingling and numbness would come and go and pain in my neck from the surgery site did not subside, even after my physical therapy was completed.
I figured that the healing process would take a great deal of time given the levels of fusion, so it wasn’t taking much of a precedent in my life. Work was going well and I was enjoying meeting new people from all over the country and all walks of life.
My girlfriend and I were settling into a comfortable life in Austin. The transition from Indianapolis was difficult, but slowly our routine and habits took hold.
However, the pain in my lower back, legs, and neck did not decrease with time. It was getting really bad. My sleep patterns started to suffer again (similar to life before and after my first back surgery). The insomnia from the pain was impacting every part of my life. I was getting grumpy and short tempered. My patience in dealing with small tasks was waning. It was time to go back to the neurosurgeon.
The doctor prescribed some follow-up x-rays and assured me that the union with the cadaver bones was progressing. I wasn’t so sure so I did some research and made appointments to see another neurosurgeon and an orthopedic spinal surgeon for second opinions.
After seeing both doctors, they both independently agreed that my neck was not fusing and that I was one of the lucky 5%-20% whose body is not compatible with cadaver bones. ARRGGHHH!!!!!
“When you come to the end of your rope, tie a knot and hang on.”
Franklin D. Roosevelt
All of my experience with doctors of multiple disciplines allowed me to gauge their bedside manners and opinions. It is very interesting to see the differences between neurosurgeons and orthopedic spinal surgeons. In my experience, it seems that if neurosurgeons feel that they can’t fix a problem, then no other doctor will be able to fix it. And it makes some sense given the amount of education and prestige bestowed upon their specialty. The “God” factor seems to come into play.
Orthopedic spinal surgeons take a more complete and practical approach to addressing a health issue. It is not just about performing surgery, then if that doesn’t work, sending a patient to a pain clinic. It is about doing as much as possible through physical therapy, targeted medications, and less invasive techniques before even considering surgery.
This was the reason that I choose to work with orthopedic spinal surgeons instead of neurosurgeons. Plus, I have been blessed to be patients of some of the best orthopedic specialists in the country who are not only gifted doctors, but also wonderful people.
Following the appointments to gather second and third opinions on my spine, I decided to work with a spinal surgery practice in Austin (after much discussion and research). The doctor ordered another battery of tests, including x-rays, CT scans, bone scans, EEG’s, EMG’s, CT myelograms (which really suck), and a number of other acronyms that I can’t remember.
If I was to say that one test is worse than any other, it would be the CT myelogram. The test requires you to lie on your stomach while contrast dye is injected into the sac that surrounds your spinal cord. Your body is tilted so that the dye can flow to the necessary part of the spine while pictures are taken by the CT scanner. The injections aren’t fun and my reaction to the dye was pretty bad (night terrors and paralysis, terrible mood swings), but this first injection process was truly memorable. The intent was for the injection to be mad in my lumbar region then tilt my body to move the dye throughout my spine. However, the doctor had a problem getting the needle between my vertebrae and into the spinal sac, so he tried another spot. Then another. Then another. I distinctly remember looking to the side and seeing the doctor’s hands shaking because he was pushing the needle so hard. I then picked up my head to look at the nurse and she had her hands over her eyes because she didn’t want to look at the doctor’s attempts. After multiple attempts, they took me off the table and performed a CT scan on my back in an attempt to find a hole for the needle. They finally found a spot and performed the test, but only after I had over 20 needle marks in my back. What we did not know was that my ligaments had calcified around my entire lumbar region so it was one large mass of bone. But that is why the tests are run.
Remember, these tests are necessary evils in order for the doctors to get a detailed view of my spine. I will go through these tests (albeit not happily) for accurate diagnoses to be made. But, oy…..not fun.
At the follow-up doctor’s appointment, the doctor said, “Doug, you have a really bad back.” And then proceeded to outline the coming challenges that I was about to face. His demeanor was honest, up front, and caring.
The doctor had two primary concerns. First was that my neck was not fusing from my prior surgery. It was the reason for the residual pain at the surgery site as well as down my arms. Second, and most importantly, the lumbar region was in worse shape than my cervical spine. As noted in the test results, my lower back was a complete block of bone. The discs were all but gone and the stenosis was evident at just about every level. This was causing the pain in my lower back and legs. But it was more serious than the pain because the impingement was severe enough to restrict blood supply to the nerves. There was significant potential to have permanent nerve damage if my spine was not corrected soon.
The doctor likened the scenario to when you sleep the wrong way or sit improperly for an extended period of time and your arm or leg falls asleep. Now imagine this happens for years. Nerves become damaged or completely die. This is not a good situation.
The orthopedic surgeon described the surgery in detail. It was going to be an anterior and posterior procedure. A vascular surgeon would be making a four inch incision starting at the bottom of my belly button and working upwards. He would move all the squishy organs aside so that the orthopedic surgeon could implant screws and plates into my L4-L5-S1 vertebrae. The vascular surgeon would close me up, then I would be turned over so that a similar incision could be made in the opposite side of my back and the same screws and plates inserted. This would give me more stability given my larger body size.
It was imperative that I get my body in shape for this serious surgery, especially my legs, so I started intensive physical therapy as quickly as possible. Three times a week with the therapists, plus doing the same exercises at home, improved my body strength quickly. I can’t stress how important this was for both my physical and mental well-being. This same preparation was an integral part of every one of my surgeries and helped my through each recovery.
The surgery was scheduled for September of 2009. One of the first things that I remember following the surgery was my orthopedic surgeon saying to me, “Doug, your surgery kicked my ass!” It ended up being a 7 ½ hour procedure. The doctor had to literally break apart my vertebrae in order to restore movement and insert the screws and plates. The pressure on the impingement was relieved in my nerve roots and I had had two vertebral fractures that also contributed to a lot of my pain.
I was in the hospital for 4 days, and it was a good time. After I was discharged, I ended up contracting double pneumonia as a result of aspirating into my lungs and spent another 5 days in the hospital. At least I was able to get personalized physical therapy.
I returned to work after about 4 weeks of physical therapy. It was painful but it felt good to be back in the swing of things. My lower back was still in the initial healing process but my neck continued to give me problems.
My orthopedic surgeon referred me to a colleague due to the severe degradation of my entire spine. This would give me the best chance of recovery and improvement in my quality of life.
“When the world says, ‘Give up,’ hope whispers, ‘Try it one more time.’"
Author Unknown
My new orthopedic surgeon was a specialist in all forms of scoliosis, and specifically, Scheuermann’s Disease. The initial consultation went very well. He was very personable and honest, but most importantly, was a fellow University of Pittsburgh graduate!
It was too early to determine the degree of fusion in my lower back, so my doctor wanted to concentrate on fixing my cervical spine. It was obvious that the initial surgery was not successful, so he determined the best route to go would be to perform a redo of my cervical fusion, which included:
The surgery was going to be very intense and dangerous due to the length of time needed to complete the procedure (projected at 8 hours) and severity of the spinal degradation. However, this was necessary to maintain use and function of my arms as well as to arrest further disc/vertebral bone loss. It was a scary proposition but there was little choice in the matter.
My cervical/thoracic revision was performed in February of 2010. I arrived at the hospital bright and early at 5:30am for the 7:00am procedure. The doctor was going to notify my girlfriend when the surgery was completed so she went back to work following my hospital admission.
Evidently, my procedure did not go completely as planned. I have a very high tolerance to narcotics, so the amount of sedatives needed to put me under anesthesia were significant. The nurses were not able to wake me up after the surgery so I spent a great deal of time in the ICU.
I woke up in ICU a number of hours later to the most excruciating pain that anyone can ever imagine. My doctor does not permit the use of pain medications immediately following surgery so that my motor function can be verified. This means that I felt every single thing done to my skin, bone, muscles, and nerves. I can remember laying on the gurney with tears running down my face as the nurses completed their check of my nerves. Then, as they applied the pain medication, my tolerance was so high due to the number of surgeries that it seemed to take forever for their effect to be felt.
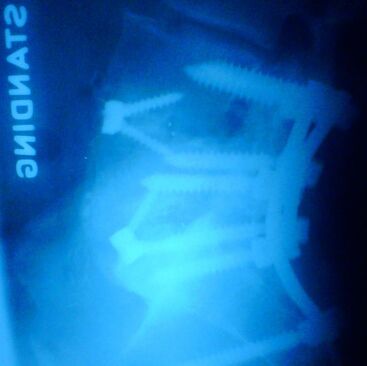
Below are photos of the first cervical/thoracic revision.
However, there have been some prescriptions that seem to work the best for me: NSAID’s (non-steroidal anti-inflammatory drugs). There are some risks in taking these drugs but they take the edge off the constant pain and make me less grumpy. However, I can’t take these after spinal fusion surgeries since the bones need the inflammation to fuse properly. This poses a problem given the number of my spinal fusions over the last 4 years (as described in the following text).
But you never plan or prepare for the day when the simplest activities cause excruciating pain. Walking, sitting, sleeping, or standing (oh man, standing stationary was, and still is, the WORST pain) became so difficult that it was almost impossible to make it through a workday. That was the catalyst for me to seek out medical professionals in neurology as well as spinal orthopedics.
I met with a number of different specialists and chose to work with an excellent neurosurgeon in Indianapolis. The doctor ordered a number of spinal tests: CT scan, x-rays, and MRI so that the extent of my degeneration could be assessed. Our first appointment was very memorable as we discussed the test results. He told me that the degeneration was extensive in my entire spine and the x-rays looked like they were from someone 30 years my elder! It wasn’t that the comment was surprising, it was just that I was expecting this happen when I was much older, not in my early 30’s.
The doctor recommended different treatments before any surgical procedure was considered. The first non-invasive treatment was the use of traction. This involved me lying on a special table on my back, (the table was similar to that in a massage therapist’s room). They strapped me onto the table with a belt affixed around my waist. Weights were placed onto a pulley system which was in turn attached to the waist belt. Progressively higher weights were added to the pulleys which then pulled on my legs to help decompress the spine. Unfortunately, I lost the feeling in my left foot after a few treatments so the doctor recommended that the traction cease.
The next step on the treatment trail was injection of cortisone into the inflamed nerves in my lumbar spine. If that sounds fun, then you are right. The shots weren’t like getting a flu vaccine in your arm. Evidently it is important to inject the inflamed nerve vveerryy sslloowwllyy with the cortisone. I will never forget the look on my doctor’s face when I turned around and looked at him with sweat on my brow and said, “You are never doing that to me again.” Thought he was going to immediately bolt out of the room.
The cortisone was intended to relieve some of the inflammation and pain in my nerve, but any relief was short-lived as the pain quickly returned within hours. My doctor and I then discussed the next level of treatment, which was to attempt to relieve the pain from the foraminal stenosis in my lower back. As the vertebral canals (containing the nerves controlling the leg movement and sensation) narrowed, pressure was being placed on the nerve roots causing pain. This was starting to significantly alter my life, from unending insomnia to limited activity and movement. At the time, I was living in Indianapolis and did not have any family living nearby. Thankfully, my wonderful family came to the rescue.
With the operation quickly approaching, my parents (both in their 70’s) made the trip from Pittsburgh to Indianapolis to help me during the surgery and recovery process. Somewhat embarrassing for a grown man in his 40’s to have his parents take care of him, but thank God they were there to help.
The goal of the surgery was to remove bone in the lumbar canal that was pressing on my nerve roots. This, in turn, would hopefully relieve the pain and improve motor function.
The day of the operation, my parents waited patiently for word from the neurosurgeon. Finally, he appeared in the waiting room and informed my parents that my nerve roots (L5) were just “smashed” from the narrowing of the spinal canal. Fortunately, the doctor was able to expand the vertebral canal and relieve some of the pressure on my nerve roots, but only time would tell if the surgery was successful.
Recovery was slow and painful. My parents stayed with me for about a week, then my awesome sister made the trek to Indianapolis to help me for another week. She showed the patience of a saint in taking care of me for that week. I was a little grumpy to say the least. My family has been so supportive, what a true blessing.
My employer was amazingly generous and understanding as I limped my way back to work after a couple of weeks. People would often find me lying down on my office floor reading because being upright was so painful.
The purpose behind explaining the treatment and therapy process is that I don’t want anyone to think that surgery was thought of lightly. I delayed this invasive procedure as long as possible. I know there are people out there living with SK and are considering surgery, so don’t feel that you are alone in the quandary. As my doctors have always told me, treatment varies by person and only you can make an informed decision that is best for you.
“I learned a long time ago that minor surgery is when they do the operation on someone else, not you.”
Bill Walton
I eventually made a partial recovery but the pain persisted and my physical activities still had to be curtailed. Not long after the surgery, my employer was bought out 2 times in 6 weeks and my position at the bank was eliminated. Our awesome team of financial services professionals quietly moved to other jobs or companies. I found myself out of work and the pain was increasing daily.
I was fortunate to find work quickly and started work with an exceptional employer in Austin, TX. This job required relocation to Austin and travel on a weekly basis (mostly flying). I figured that I could deal with the pain of being on the road again and felt fortunate to have the opportunity to work for such a successful company. So my girlfriend and I packed up the two cats and headed for Texas.
Traveling nationally for work was more of a pain than expected, literally. Sitting in a cramped space for hours on end proved to be a real challenge. The pain was mostly in my lower back and legs. A sharp, needle like pain in my lumbar region that radiated down both legs. It got so bad sometimes that I was drenched in sweat by the time the plane landed. Plus, security procedures following 9/11 (both my brother and I were on planes that terrible morning in 2001 that were forced to land) made waiting times on the tarmac longer, which increased my pain. Necessary steps given the scary world of the 21st century, but difficult to weather with the pain.
Work was going well and we were adjusting to our new lives as Texans. I continued to travel weekly and was mostly able to keep my workout routine of 3 times a week. The workouts included light weight and elliptical training which not only relieved stress but also improved my mobility.
It was after about a year of this routine when I noticed that my arms and hands became numb and tingly after workouts. The numbness got so bad that I couldn’t open the locker or car door immediately following training. I figured that given my past shoulder problems that I slept wrong and just pinched some nerves.
After a while of dealing with the arm and hand sensations, I scheduled an appointment with a rheumatologist in Austin. The medical files from my doctors in Indianapolis were forwarded to the rheumatologist and we had an initial consult. The doctor ordered some tests and we scheduled another appointment to discuss the results.
This next appointment was a turning point in my medical life as the doctor said that there was nothing that he could do to help me. He recommended that I see a neurosurgeon as there were significant problems with my entire spine. However, he said that the primary focus was to be my cervical area. This came as a shock since my neck never really gave me that many problems. Sure it was stiff most of the time, but hey, who doesn’t have a stiff neck?
I then consulted with a recommended neurosurgeon who ordered some additional tests. The results were shocking. There were little, if any, discs remaining in most of my neck. The discs were almost completely gone between C3 and C6. This was the cause of my arm and hand sensations and hopefully the nerve damage would not be permanent. The recommendation was immediate fusion of C3-C6 with the use of cadaver bones. An incision would be made through my throat with screws and plates inserted on the anterior, or inside, of my spine to hold it secure until fusion occurred. I would be in a cervical collar for about 3 months and travel would be curtailed until then.
My employer was notified and they were GREAT about it. Their major concern was for my health and they encouraged me to do what I needed to get better.
So, I went in for surgery in June of 2008 and had the C3-C6 fusion surgery. My stay in the hospital short and 2 days later I was home resting uncomfortably. After 3 weeks I was back to work at a desk job until the neurosurgeon cleared me to travel. Wearing the cervical collar 24 hours a day was a pain in the butt, but necessary.
Three months later, work travel resumed and I was back in the swing of things. Physical therapy, including deep tissue massage, was begun and progress was slow and tedious.
It was great getting back to my full work schedule, both mentally and physically. Being up and around made me feel alive again, but there was still some lingering effects of the nerve damage to my arms. The tingling and numbness would come and go and pain in my neck from the surgery site did not subside, even after my physical therapy was completed.
I figured that the healing process would take a great deal of time given the levels of fusion, so it wasn’t taking much of a precedent in my life. Work was going well and I was enjoying meeting new people from all over the country and all walks of life.
My girlfriend and I were settling into a comfortable life in Austin. The transition from Indianapolis was difficult, but slowly our routine and habits took hold.
However, the pain in my lower back, legs, and neck did not decrease with time. It was getting really bad. My sleep patterns started to suffer again (similar to life before and after my first back surgery). The insomnia from the pain was impacting every part of my life. I was getting grumpy and short tempered. My patience in dealing with small tasks was waning. It was time to go back to the neurosurgeon.
The doctor prescribed some follow-up x-rays and assured me that the union with the cadaver bones was progressing. I wasn’t so sure so I did some research and made appointments to see another neurosurgeon and an orthopedic spinal surgeon for second opinions.
After seeing both doctors, they both independently agreed that my neck was not fusing and that I was one of the lucky 5%-20% whose body is not compatible with cadaver bones. ARRGGHHH!!!!!
“When you come to the end of your rope, tie a knot and hang on.”
Franklin D. Roosevelt
All of my experience with doctors of multiple disciplines allowed me to gauge their bedside manners and opinions. It is very interesting to see the differences between neurosurgeons and orthopedic spinal surgeons. In my experience, it seems that if neurosurgeons feel that they can’t fix a problem, then no other doctor will be able to fix it. And it makes some sense given the amount of education and prestige bestowed upon their specialty. The “God” factor seems to come into play.
Orthopedic spinal surgeons take a more complete and practical approach to addressing a health issue. It is not just about performing surgery, then if that doesn’t work, sending a patient to a pain clinic. It is about doing as much as possible through physical therapy, targeted medications, and less invasive techniques before even considering surgery.
This was the reason that I choose to work with orthopedic spinal surgeons instead of neurosurgeons. Plus, I have been blessed to be patients of some of the best orthopedic specialists in the country who are not only gifted doctors, but also wonderful people.
Following the appointments to gather second and third opinions on my spine, I decided to work with a spinal surgery practice in Austin (after much discussion and research). The doctor ordered another battery of tests, including x-rays, CT scans, bone scans, EEG’s, EMG’s, CT myelograms (which really suck), and a number of other acronyms that I can’t remember.
If I was to say that one test is worse than any other, it would be the CT myelogram. The test requires you to lie on your stomach while contrast dye is injected into the sac that surrounds your spinal cord. Your body is tilted so that the dye can flow to the necessary part of the spine while pictures are taken by the CT scanner. The injections aren’t fun and my reaction to the dye was pretty bad (night terrors and paralysis, terrible mood swings), but this first injection process was truly memorable. The intent was for the injection to be mad in my lumbar region then tilt my body to move the dye throughout my spine. However, the doctor had a problem getting the needle between my vertebrae and into the spinal sac, so he tried another spot. Then another. Then another. I distinctly remember looking to the side and seeing the doctor’s hands shaking because he was pushing the needle so hard. I then picked up my head to look at the nurse and she had her hands over her eyes because she didn’t want to look at the doctor’s attempts. After multiple attempts, they took me off the table and performed a CT scan on my back in an attempt to find a hole for the needle. They finally found a spot and performed the test, but only after I had over 20 needle marks in my back. What we did not know was that my ligaments had calcified around my entire lumbar region so it was one large mass of bone. But that is why the tests are run.
Remember, these tests are necessary evils in order for the doctors to get a detailed view of my spine. I will go through these tests (albeit not happily) for accurate diagnoses to be made. But, oy…..not fun.
At the follow-up doctor’s appointment, the doctor said, “Doug, you have a really bad back.” And then proceeded to outline the coming challenges that I was about to face. His demeanor was honest, up front, and caring.
The doctor had two primary concerns. First was that my neck was not fusing from my prior surgery. It was the reason for the residual pain at the surgery site as well as down my arms. Second, and most importantly, the lumbar region was in worse shape than my cervical spine. As noted in the test results, my lower back was a complete block of bone. The discs were all but gone and the stenosis was evident at just about every level. This was causing the pain in my lower back and legs. But it was more serious than the pain because the impingement was severe enough to restrict blood supply to the nerves. There was significant potential to have permanent nerve damage if my spine was not corrected soon.
The doctor likened the scenario to when you sleep the wrong way or sit improperly for an extended period of time and your arm or leg falls asleep. Now imagine this happens for years. Nerves become damaged or completely die. This is not a good situation.
The orthopedic surgeon described the surgery in detail. It was going to be an anterior and posterior procedure. A vascular surgeon would be making a four inch incision starting at the bottom of my belly button and working upwards. He would move all the squishy organs aside so that the orthopedic surgeon could implant screws and plates into my L4-L5-S1 vertebrae. The vascular surgeon would close me up, then I would be turned over so that a similar incision could be made in the opposite side of my back and the same screws and plates inserted. This would give me more stability given my larger body size.
It was imperative that I get my body in shape for this serious surgery, especially my legs, so I started intensive physical therapy as quickly as possible. Three times a week with the therapists, plus doing the same exercises at home, improved my body strength quickly. I can’t stress how important this was for both my physical and mental well-being. This same preparation was an integral part of every one of my surgeries and helped my through each recovery.
The surgery was scheduled for September of 2009. One of the first things that I remember following the surgery was my orthopedic surgeon saying to me, “Doug, your surgery kicked my ass!” It ended up being a 7 ½ hour procedure. The doctor had to literally break apart my vertebrae in order to restore movement and insert the screws and plates. The pressure on the impingement was relieved in my nerve roots and I had had two vertebral fractures that also contributed to a lot of my pain.
I was in the hospital for 4 days, and it was a good time. After I was discharged, I ended up contracting double pneumonia as a result of aspirating into my lungs and spent another 5 days in the hospital. At least I was able to get personalized physical therapy.
I returned to work after about 4 weeks of physical therapy. It was painful but it felt good to be back in the swing of things. My lower back was still in the initial healing process but my neck continued to give me problems.
My orthopedic surgeon referred me to a colleague due to the severe degradation of my entire spine. This would give me the best chance of recovery and improvement in my quality of life.
“When the world says, ‘Give up,’ hope whispers, ‘Try it one more time.’"
Author Unknown
My new orthopedic surgeon was a specialist in all forms of scoliosis, and specifically, Scheuermann’s Disease. The initial consultation went very well. He was very personable and honest, but most importantly, was a fellow University of Pittsburgh graduate!
It was too early to determine the degree of fusion in my lower back, so my doctor wanted to concentrate on fixing my cervical spine. It was obvious that the initial surgery was not successful, so he determined the best route to go would be to perform a redo of my cervical fusion, which included:
- Leaving the anterior cervical screws and plates in my neck from my first surgery.
- Entering my spine via the back (posterior).
- Increasing the fusion levels from C2-T2 due to the spreading severe disc degradation.
- Utilize bone fragments scraped from my cervical spine during surgery and mixed with BMP (a new grafting material called Bone Morphogenic Protein) to improve the likelihood of fusion.
The surgery was going to be very intense and dangerous due to the length of time needed to complete the procedure (projected at 8 hours) and severity of the spinal degradation. However, this was necessary to maintain use and function of my arms as well as to arrest further disc/vertebral bone loss. It was a scary proposition but there was little choice in the matter.
My cervical/thoracic revision was performed in February of 2010. I arrived at the hospital bright and early at 5:30am for the 7:00am procedure. The doctor was going to notify my girlfriend when the surgery was completed so she went back to work following my hospital admission.
Evidently, my procedure did not go completely as planned. I have a very high tolerance to narcotics, so the amount of sedatives needed to put me under anesthesia were significant. The nurses were not able to wake me up after the surgery so I spent a great deal of time in the ICU.
I woke up in ICU a number of hours later to the most excruciating pain that anyone can ever imagine. My doctor does not permit the use of pain medications immediately following surgery so that my motor function can be verified. This means that I felt every single thing done to my skin, bone, muscles, and nerves. I can remember laying on the gurney with tears running down my face as the nurses completed their check of my nerves. Then, as they applied the pain medication, my tolerance was so high due to the number of surgeries that it seemed to take forever for their effect to be felt.
Below are photos of the first cervical/thoracic revision.
Even though the pain was bad it was nothing like what my girlfriend had to endure. She was expecting to see me in recovery in the early afternoon on the day of surgery. However, due to complications, I spent a long time in ICU recovery and she did not receive a call until late in the day. She arrived in the waiting area about 7pm and kept asking about my condition but the only news that she received was that I was still in recovery. Finally, at about 10:30pm, she got news that I was in the Intermediate Unit and that she could finally see me. Thought she was going to have a coronary when I first saw her. God love her……….
I was up and walking the day after surgery and overall spent about 5 days in the hospital. Physical therapy couldn’t start for a minimum of 6 months following surgery so I laid low and was back to work in a couple months, cervical/thoracic brace and all.
“I think music in itself is healing. It's an explosive expression of humanity. It's something we are all touched by. No matter what culture we're from, everyone loves music.”
Billy Joel
While at work, I noticed that I started to have seriously painful headaches. These started immediately following the surgery but I thought they were just from the healing process. The pain wouldn’t let up, 24 hours a day. Other symptoms included nausea, one of my eyes turned red and the eyelid drooped, my pulse pounded in my temple, my ears rang, and my skin flushed when the pain was really bad (which was all the time). After about 2 months of pain and being grumpy, I finally went to my family doctor where I was diagnosed with Hoskin’s Syndrome, or cluster headaches. These feel like someone is relentlessly squeezing your head in a vice. I have my share of bad headaches in the past, but these are different. The doctor was able to alleviate some of the pain with cortisone injections into my neck and prescribed Lidocaine patches. These patches were to be applied to my neck when the pain was getting unbearable but the pain would come back once the patches are removed. Honestly, these things do work for me and help relieve some of the pain, but the headaches never really leave. Small price to pay……
As was previously mentioned, my job required significant travel (mostly via air), so I was back on board a plane as soon as it was approved by my doctor. My neck was in the healing process and would take months to determine the level of fusion. However, it seemed that my lower back wasn’t getting any better.
The pain in my lower back worsened and it was becoming increasingly difficult to walk. There is nothing like being stuck on the runway in Jackson Hole, WY while in so much pain that the sweat drips down your face and your shirt is plastered to your body. Not complaining, mind you. I was fortunate to be walking let alone flying in a plane.
Day by day, week by week, it became more difficult to keep my train of thought and concentration. Regardless of the task at hand, or the position of my body, the pain in my lower back and down my legs never receded.
After the first follow-up appointment with the orthopedic surgeon for my neck surgery, he said that it was too early to tell if it was successful but he was concerned about my lower back. He then ordered another CT myelogram to determine the level of bone grafting in my L4-L5-S1.
The results came in and I went to see the doctor so we could decide the next step. The CT myelogram noted some fusion between L4 and L5 but there was no indication that the grafting was taking place at L5-S1. This could be the cause of the surgery site discomfort and the radiating pain down my legs. We decided that the best thing to do would be to fix this non-union. The doctor needed to perform surgery and replace the existing hardware with sturdier screws and rods. He also was going to save as much bone from my spine during the procedure as he could while taking the bone from my remaining pelvic iliac crest. He would add BMP to this bone and pack the site as tightly as possible so it gave me the best chance for fusion.
The revision was performed in September 2010. Fortunately, it was only a posterior, or through the back, redo so the recovery process would not be as long as the first lumbar fusion. Below are photos of the surgery.
I was up and walking the day after surgery and overall spent about 5 days in the hospital. Physical therapy couldn’t start for a minimum of 6 months following surgery so I laid low and was back to work in a couple months, cervical/thoracic brace and all.
“I think music in itself is healing. It's an explosive expression of humanity. It's something we are all touched by. No matter what culture we're from, everyone loves music.”
Billy Joel
While at work, I noticed that I started to have seriously painful headaches. These started immediately following the surgery but I thought they were just from the healing process. The pain wouldn’t let up, 24 hours a day. Other symptoms included nausea, one of my eyes turned red and the eyelid drooped, my pulse pounded in my temple, my ears rang, and my skin flushed when the pain was really bad (which was all the time). After about 2 months of pain and being grumpy, I finally went to my family doctor where I was diagnosed with Hoskin’s Syndrome, or cluster headaches. These feel like someone is relentlessly squeezing your head in a vice. I have my share of bad headaches in the past, but these are different. The doctor was able to alleviate some of the pain with cortisone injections into my neck and prescribed Lidocaine patches. These patches were to be applied to my neck when the pain was getting unbearable but the pain would come back once the patches are removed. Honestly, these things do work for me and help relieve some of the pain, but the headaches never really leave. Small price to pay……
As was previously mentioned, my job required significant travel (mostly via air), so I was back on board a plane as soon as it was approved by my doctor. My neck was in the healing process and would take months to determine the level of fusion. However, it seemed that my lower back wasn’t getting any better.
The pain in my lower back worsened and it was becoming increasingly difficult to walk. There is nothing like being stuck on the runway in Jackson Hole, WY while in so much pain that the sweat drips down your face and your shirt is plastered to your body. Not complaining, mind you. I was fortunate to be walking let alone flying in a plane.
Day by day, week by week, it became more difficult to keep my train of thought and concentration. Regardless of the task at hand, or the position of my body, the pain in my lower back and down my legs never receded.
After the first follow-up appointment with the orthopedic surgeon for my neck surgery, he said that it was too early to tell if it was successful but he was concerned about my lower back. He then ordered another CT myelogram to determine the level of bone grafting in my L4-L5-S1.
The results came in and I went to see the doctor so we could decide the next step. The CT myelogram noted some fusion between L4 and L5 but there was no indication that the grafting was taking place at L5-S1. This could be the cause of the surgery site discomfort and the radiating pain down my legs. We decided that the best thing to do would be to fix this non-union. The doctor needed to perform surgery and replace the existing hardware with sturdier screws and rods. He also was going to save as much bone from my spine during the procedure as he could while taking the bone from my remaining pelvic iliac crest. He would add BMP to this bone and pack the site as tightly as possible so it gave me the best chance for fusion.
The revision was performed in September 2010. Fortunately, it was only a posterior, or through the back, redo so the recovery process would not be as long as the first lumbar fusion. Below are photos of the surgery.
It was pretty painful but I was getting “old hat” at this. I was well versed in the recuperation process so I was up and walking the day after surgery. This was so important not only for my mental well-being, but also for my internal health. The anesthesia and pain medications administered in the hospital play havoc with one’s digestive process. In other words they tend to make a person extremely constipated! This only adds to the pain of the surgery and delays being released from the hospital. As usual, they wouldn’t discharge me until I made a bowel movement. Getting upright as soon as possible allows gravity to hold and speeds up the pooping process so I was all over standing up and walking immediately.
I was home and resting after 4 days in the hospital, walker and all (although I only used the walker for a couple of days). The recovery process was about the same: lots of sleep and rest and walking daily. My appetite isn’t the best following the surgeries due to the medication and pain, so I drink Carnation Instant Breakfast daily to keep my energy level up.
I wore a lumbar brace that was pretty cumbersome, but necessary to stabilize the surgery site. My days were filled with sitting in a recliner listening to music or reading, anything to get your mind off of the pain.
I started having severe diaphragm cramps (and still have them today) right after the surgery. They would appear just under each side of my ribcage, last for anywhere from 5 to 30 minutes, and felt like someone was stabbing me in the stomach. The doctor felt that it was my stomach muscles going into spasm from lack of use due to the brace. They seemed to end more quickly if I drank tonic water when they started.
The days seemed to drag into one long recovery process. I kept as busy as possible but being upright for any length of time increased the pain. Reading books and surfing the net were ways to pass the time, but my arms started shaking and quivering while my fingers tingled and went numb after only a couple of minutes. This made the days really long and I refused to turn on the television until late in the afternoon. I wasn’t going to let my mind go numb by watching television all day.
My follow-up appointment with the orthopedic went well. Initial x-rays were promising but he was very concerned about the sensations going down my arms so he ordered another EMG (electromyography: when they stick a needle into your muscles and hook it up to a machine that assesses the electrical activity) and dreaded CT myelogram. There was a potential for non-union of the lower sections of my cervical spine and upper portions of my thoracic spine, so he wanted to make sure that all was well.
A couple weeks later I was in the doctor’s office for the results and they were a mixed bag. The good news was that my neck was fusing!!! The use of my own bone, in place of cadaver bones, in addition to the BMP was working. What a relief! On the other hand, there were indications that the lower areas of my neck surgical site (lower cervical and upper thoracic) were not grafting. This could be due to a number of reasons, but it was correctible.
See, since I am a larger person, the screws and rods implanted into my C7-T1-T2 were not sturdy enough for my frame. The doctor placed a special order to a medical device company to create new rods and screws that were made of cobalt chrome instead of titanium. This new hardware was sturdier and would better suit my larger body.
Five months after my lower back revision, the new cobalt chrome screws and rods were completed and surgery was schedule for my 2nd neck revision in February of 2011. The new hardware was going to be implanted to replace the titanium screws and rods and would potentially correct the quivering and tingling in my fingers and hands. The doctor would also be able to determine the degree of grafting success in my cervical spine by reopening the former surgical site and testing the density of the new bone growth.
As before, I went into the hospital in February of 2011 and had the second cervical/thoracic fusion revision. The surgery lasted 5 ½ hours and went smoothly with the exception of the initial post-operative recovery. Evidently I had a little bit more trouble with the anesthetic as I was building up tolerance to the medication. They administered a great deal of the anesthesia to put me under, but that complicated my ability to recover quickly so I spent a number of hours in ICU as my breathing stopped sporadically. But after a while, I was back into the Intermediate Care Unit with my girlfriend at my side. It was a little scary but I survived.
Below are photos of my second neck (cervical/thoracic) spinal revision.
I was home and resting after 4 days in the hospital, walker and all (although I only used the walker for a couple of days). The recovery process was about the same: lots of sleep and rest and walking daily. My appetite isn’t the best following the surgeries due to the medication and pain, so I drink Carnation Instant Breakfast daily to keep my energy level up.
I wore a lumbar brace that was pretty cumbersome, but necessary to stabilize the surgery site. My days were filled with sitting in a recliner listening to music or reading, anything to get your mind off of the pain.
I started having severe diaphragm cramps (and still have them today) right after the surgery. They would appear just under each side of my ribcage, last for anywhere from 5 to 30 minutes, and felt like someone was stabbing me in the stomach. The doctor felt that it was my stomach muscles going into spasm from lack of use due to the brace. They seemed to end more quickly if I drank tonic water when they started.
The days seemed to drag into one long recovery process. I kept as busy as possible but being upright for any length of time increased the pain. Reading books and surfing the net were ways to pass the time, but my arms started shaking and quivering while my fingers tingled and went numb after only a couple of minutes. This made the days really long and I refused to turn on the television until late in the afternoon. I wasn’t going to let my mind go numb by watching television all day.
My follow-up appointment with the orthopedic went well. Initial x-rays were promising but he was very concerned about the sensations going down my arms so he ordered another EMG (electromyography: when they stick a needle into your muscles and hook it up to a machine that assesses the electrical activity) and dreaded CT myelogram. There was a potential for non-union of the lower sections of my cervical spine and upper portions of my thoracic spine, so he wanted to make sure that all was well.
A couple weeks later I was in the doctor’s office for the results and they were a mixed bag. The good news was that my neck was fusing!!! The use of my own bone, in place of cadaver bones, in addition to the BMP was working. What a relief! On the other hand, there were indications that the lower areas of my neck surgical site (lower cervical and upper thoracic) were not grafting. This could be due to a number of reasons, but it was correctible.
See, since I am a larger person, the screws and rods implanted into my C7-T1-T2 were not sturdy enough for my frame. The doctor placed a special order to a medical device company to create new rods and screws that were made of cobalt chrome instead of titanium. This new hardware was sturdier and would better suit my larger body.
Five months after my lower back revision, the new cobalt chrome screws and rods were completed and surgery was schedule for my 2nd neck revision in February of 2011. The new hardware was going to be implanted to replace the titanium screws and rods and would potentially correct the quivering and tingling in my fingers and hands. The doctor would also be able to determine the degree of grafting success in my cervical spine by reopening the former surgical site and testing the density of the new bone growth.
As before, I went into the hospital in February of 2011 and had the second cervical/thoracic fusion revision. The surgery lasted 5 ½ hours and went smoothly with the exception of the initial post-operative recovery. Evidently I had a little bit more trouble with the anesthetic as I was building up tolerance to the medication. They administered a great deal of the anesthesia to put me under, but that complicated my ability to recover quickly so I spent a number of hours in ICU as my breathing stopped sporadically. But after a while, I was back into the Intermediate Care Unit with my girlfriend at my side. It was a little scary but I survived.
Below are photos of my second neck (cervical/thoracic) spinal revision.
This time I was up and around quickly so my hospital stay only lasted 3 days. I went home with the help of my girlfriend (who, by the way, has earned her wings into heaven!!) to recuperate, but this time, wearing two braces. I continued to wear my lumbar brace but also had to wear the cervical/thoracic collar. They weren’t the most comfortable but were needed in order to keep my spine sedentary.
I was in both braces for about 3 ½ months (from February-May), as you can see from the photo below.
I was in both braces for about 3 ½ months (from February-May), as you can see from the photo below.
"In reality, hope is the worst of all evils, because it prolongs man's torments."
Friedrich Nietzsche, Human, All Too Human, 1878
This quote goes to show you that Nietzsche was a bloomin’ pessimistic idiot. Hope is really is the only thing that keeps some people living.
This was evident in the follow-up appointment from the 2nd neck revision as it was a mixed bag of results. After a series of x-rays, the great news was that I was released from my cervical/thoracic and lumbar braces as the fusions were working!!!! Such awesome news! There was truly a light at the end of the tunnel for me. I can’t tell you how important it is to have HOPE, after all the years of agony and surgeries. It just lights a fire under you to set goals for recovery and get back to living!
The other news was not the best. Even though the surgeries have been successful, the remainder of my lumbar and part of the thoracic spine was showing severe deterioration as a result of the Scheuermann’s Disease.
So another CT myelogram was ordered and the test administered. The probable outcome will be additional fusion of some thoracic and lumbar vertebrae but there is a light at the end of the tunnel. My orthopedic spinal surgeon is truly a genius!!! No THAT is hope.
(Remainder of experiences will be posted in site blog)My Conclusions (so far) and Thoughts
If you are not already aware, long-term chronic pain is a very difficult affliction to manage, both mentally and physically. I go from fits of self-absorption and self-pity to grand epiphanies of life’s blessings and wonders. If that seems like an unusual or strange declaration, but it is as honest as I can be in trying to explain my coping mechanisms.
Documenting my thoughts and emotions has been a great learning experience. The peaks and valleys are constantly frustrating but manageable so far. I in no way am looking to preach or infer that I have any idea about life. But the process of noting my feelings as they occur has been cathartic and surprisingly eye-opening in many ways.
"We have no right to ask when sorrow comes, "Why did this happen to me?" unless we ask the same question for every moment of happiness that comes our way."
Author Unknown
“I'd rather laugh with the sinners than cry with the saints - The sinners are much more fun”
Billy Joel
“In everyone's life, at some time, our inner fire goes out. It is then burst into flame by an encounter with another human being. We should all be thankful for those people who rekindle the inner spirit.
Albert Schweitzer
Blessed: highly favored or fortunate, characterized by happiness and good fortune
Friedrich Nietzsche, Human, All Too Human, 1878
This quote goes to show you that Nietzsche was a bloomin’ pessimistic idiot. Hope is really is the only thing that keeps some people living.
This was evident in the follow-up appointment from the 2nd neck revision as it was a mixed bag of results. After a series of x-rays, the great news was that I was released from my cervical/thoracic and lumbar braces as the fusions were working!!!! Such awesome news! There was truly a light at the end of the tunnel for me. I can’t tell you how important it is to have HOPE, after all the years of agony and surgeries. It just lights a fire under you to set goals for recovery and get back to living!
The other news was not the best. Even though the surgeries have been successful, the remainder of my lumbar and part of the thoracic spine was showing severe deterioration as a result of the Scheuermann’s Disease.
So another CT myelogram was ordered and the test administered. The probable outcome will be additional fusion of some thoracic and lumbar vertebrae but there is a light at the end of the tunnel. My orthopedic spinal surgeon is truly a genius!!! No THAT is hope.
(Remainder of experiences will be posted in site blog)My Conclusions (so far) and Thoughts
If you are not already aware, long-term chronic pain is a very difficult affliction to manage, both mentally and physically. I go from fits of self-absorption and self-pity to grand epiphanies of life’s blessings and wonders. If that seems like an unusual or strange declaration, but it is as honest as I can be in trying to explain my coping mechanisms.
Documenting my thoughts and emotions has been a great learning experience. The peaks and valleys are constantly frustrating but manageable so far. I in no way am looking to preach or infer that I have any idea about life. But the process of noting my feelings as they occur has been cathartic and surprisingly eye-opening in many ways.
"We have no right to ask when sorrow comes, "Why did this happen to me?" unless we ask the same question for every moment of happiness that comes our way."
Author Unknown
- At times, I rant and rave and am entirely self-absorbed, especially after surgery and recovery periods. It is important for me to recognize this as it happens so that I can try and stop being so selfish.
- I sometimes grieve for my loss of mobility and my new physical limitations. At night, often times I cry from the shear physical pain and insomnia. Amazing how life takes unexpected turns so quickly.
- The inability to contribute to society via work has really thrown me for a loop. I never realized how important it is for me to be a productive member of society. My work has been my life, being able to help so many people was an integral part of my being. I can’t wait to manage this pain and recovery process so that I can get back to giving.
- The brave men and women of our Armed Forces continually amaze me in their dedication to home and country. This feeling of awe has increased significantly since I have been physically beaten down by pain and surgeries and less able to take care of myself.
- I try to accept my lot in life and play the cards that I have been dealt. Believe me, it really has been a mixed bag. But what great journeys aren’t without their pitfalls? I’ve spent a great deal of time thinking in retrospect and have tried to put each phase of my life into literal terms. So far, it has gone something like this. I:
- Learned about the disease.
- Denied it would affect me.
- Understood that the previous step was bogus and unrealistic over time.
- Accepted that my life will be different.
- Assessed how my life had to change.
- Had to understand the best learning practices that I used in the past (i.e.: experience, reading, writing, note taking, repetition, etc.).
- Remember how I learned as a child, adolescent, young adult, adult.
- Understood that I always learned the same way, by doing and experiencing.
- Am working on adjusting my learning process since physical experiences are now limited.
- Set course for, and accept, whatever life has in store for me by keeping an open mind as best I can.
- At times the pain has been so bad that if feels like I am in a state of confusion. I go into a room and forget why I am there (yes, understand that it comes with age). It feels like I am in a fog and my thoughts are disjointed. My opinion is that this is not a result of prescribed medication, but rather that my sole mental focus is on the pain, not on tasks at hand. My ability to concentrate is compromised frequently, and as a result my mental acuity suffers. This often causes me to become frustrated easily and small things become enormously important. I don’t feel like going to public places or be a part of groups since my conversation skills lessen. That is a big reason why it has been so important to force myself to get out of the house and interact with people. Finding a new way to learn and stay sharp is difficult, but will be necessary for me to have any quality of life.
- Having gone through a decent amount of turmoil and pain helps me appreciate every day and realize that my life has been such a blessing. I hope that life grants me a chance to recoup some of the energy that I have wasted on selfishness so that I can give more to others. And if life does not grant me that opportunity, hopefully, then I am so thankful that I have been chosen to bear this burden as I would not wish the pain on any of my wonderful friends or family.
- I understand that as age progresses, my daily activities will become more difficult and trying. Sometimes it feels like walking up steps is like running a marathon (not that I have ever run a marathon) so I know what is in store for me down the road.
- Getting out into the sunshine helps immensely for mental and physical well-being.
“I'd rather laugh with the sinners than cry with the saints - The sinners are much more fun”
Billy Joel
- Those times that I do feel well enough to travel, I have made if a priority to travel and see those friends and family that have left a wonderful indelible print on my life.
- There were two places that were instrumental in my recovery from surgeries by providing a location that allowed me to have interaction with good people and interesting conversation. .
- First, the South Austin location of Costco was a great place to walk. I know this sounds funny, but I was home alone (in a house with steps) during my surgery recoveries and it was a concern that if I did fall that I wouldn’t receive help for hours. So, in order to get the necessary walking times completed, I would go to Costco, grab a cart, and walk the aisles. The employees were, and still are, so friendly and it gave me a sense of stability and safety. Needless to say, it wasn't the greatest on my wallet but it did me good to get out and see people. I have always been a big fan of Costco, but now I am a huge fan.
- The second place was “Black Sheep Lodge” in South Austin, TX. Maybe it is my Irish blood in me, but nothing beats a good pint of Guinness, good conversation, and good food. This place has it all, and was my sanctuary as a home away from home.
“In everyone's life, at some time, our inner fire goes out. It is then burst into flame by an encounter with another human being. We should all be thankful for those people who rekindle the inner spirit.
Albert Schweitzer
- My employer in Austin has been amazing in supporting my fight against Scheuermann’s Disease.
- Hurtful comments will be made to you from time to time (the most painful being those from friends and family). After some sleepless nights and much thought, I am learning to take these conversations in stride. I think the people that care about me have their own defense mechanisms and want me to have an improved quality of life. It has to be difficult seeing a loved one go through daily pain and suffering. Thank God I have people that love and care about me.
- Have a funny story. I went to the car dealership a while back so for some maintenance work that needed to be done on my truck. I am sitting there in the lobby when a woman 84 years young said to me, “You think you have it rough then you see someone like you”. And I am 46. We had a great conversation.
- Once my body tells me that I have been upright too long it is important that I get off my feet, so I sometimes watch television at night. It sounds strange, but a true inspiration about learning life’s lessons has come from Andrew Zimmern, the host of “Bizarre Foods” on the Travel Channel. He made it known that he spent a year being homeless and living on the streets. However, he persevered and survived to the point of becoming a popular television host. To me, this truly an inspiration as he constantly sees obstacles as a lesson to be learned.
- Living with pain is a constant reminder that we are on this world for a very short time. I live with this disease on a daily basis and there are so many people worse off than me.
- My dear friends and family continue to inspire me. Their fortitude, steadfastness, and goodness cannot be over overstated. As I said previously, my girlfriend has stuck by me every step of the way and keeps me going. She has earned her wings into heaven.
- In my world, the worst thing that can happen is to have an apathetic and indifferent view of the world. It is easy to fall into a state of depression as the pain progressively increases and both physical and mental abilities slowly diminish.
- My wish is to get back to living and have an opportunity to make a positive impact and difference……..
Blessed: highly favored or fortunate, characterized by happiness and good fortune