Very Basic Spinal Anatomy 101
|
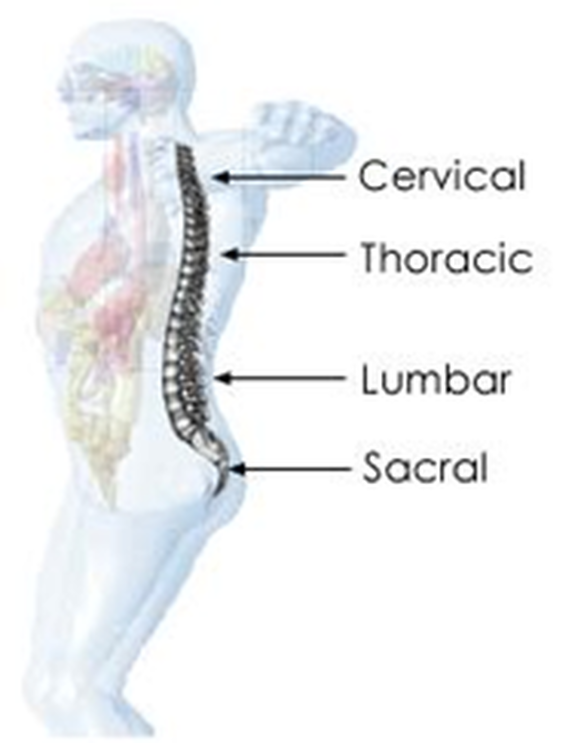
The human spine has 4 basic sections: See "Image 1"
The bones of the spine are called “vertebrae”. These vertebrae stack upon each in an interlocking manner and help protect the spinal cord. The top and the bottom of each vertebra are called the “vertebral end plates”. In between each vertebra are “discs” made up of a hard outer shell and a soft inner core. |
|
The discs act like small shock absorbers and help hold the vertebrae together.
As seen in "Image 2", a normal spine has specific curvatures:
This structure helps maintain proper body weight distribution and helps the body absorb the pounding and exertion from performing day-to-day activities. |
Historical Data
Scheuermann’s Disease was first researched by Holger Scheuermann, a Danish orthopedic surgeon, in the 1920’s. It is characterized by a “humpback” appearance and attributed to uneven growth of a person’s spinal vertebrae. It is believed to affect anywhere from .4% to 8% of the population and typically first presents itself in adolescents and teenagers.
Symptoms and Diagnosis
Scheuermann’s Disease can be diagnosed at any time in a person’s life: childhood, adolescence, or adulthood.
As a child, SD is usually identified by parents or teachers who notice a hunched posture originating in the middle, or thoracic region, of a child’s back.
Adolescents with SD usually seek medical treatment due to back pain. In addition, a high percentage these patients tend to be more active males involved in sports, heavy lifting, and may also involve sudden growth spurts during puberty.
The precursor for an adult seeing a physician is usually decreased mobility due to worsening back pain. However, the later in life the diagnosis, the higher the chance for debilitating mobility issues over time.
In order for a doctor to diagnose SD, a person must undergo a battery of tests, some of which may include:
Once the tests are read by the physician, a diagnosis of SD can include one or all of the following results:
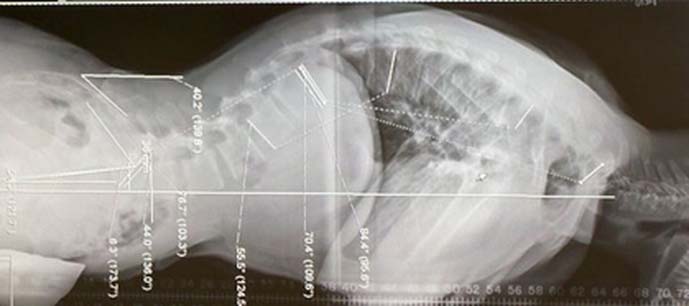
In x-rays, healthy vertebrae appear rectangular (see drop down box of healthy spine and spine with SD). However, the vertebrae of people with SD are wedge-shaped. If three or more consecutive vertebrae are wedged 5 degrees or more, then SD may be confirmed (usually in the thoracic region of the spine). The apex, or peak, of the curvature.
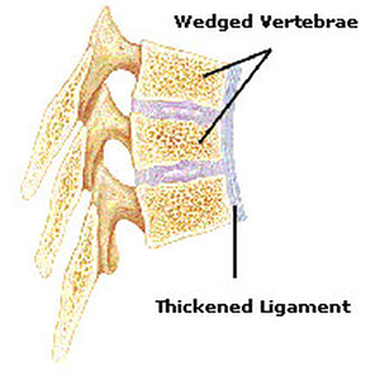
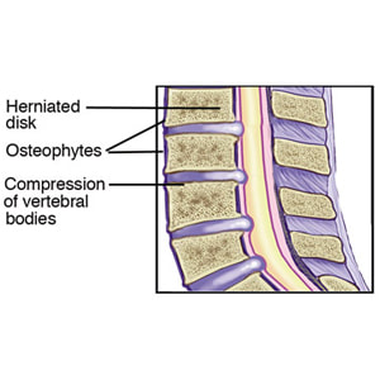
The long ligament that connects the front of the vertebra, called the anterior longitudinal ligament (see Image 3), thickens and can cause more pressure on the spine and vertebral wedging.
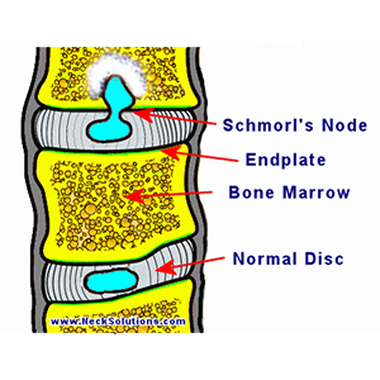
There also may be vertebral end plate irregularities, including Schmorl’s Nodes (see Image 4). These nodes appear on x-rays when disc cartilage is absorbed by, or protrudes into, the vertebral end plates. Sometimes these nodes can be so severe that SD can be misdiagnosed as infections or tumors.
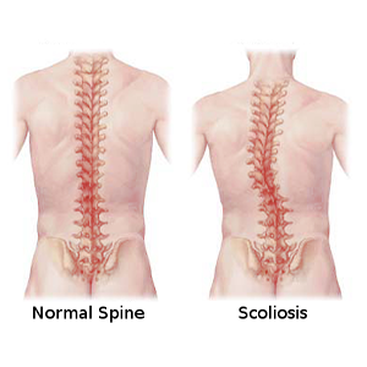
Scheuermann’s Disease differs from Scoliosis (see Image 5) in that a person with scoliosis has a sideways curve to their spine, often in an S or C shape. A patient with Scheuermann’s Disease has a curve from the front of the spine to the back, causing the aforementioned hump or “hunchback”
As a child, SD is usually identified by parents or teachers who notice a hunched posture originating in the middle, or thoracic region, of a child’s back.
Adolescents with SD usually seek medical treatment due to back pain. In addition, a high percentage these patients tend to be more active males involved in sports, heavy lifting, and may also involve sudden growth spurts during puberty.
The precursor for an adult seeing a physician is usually decreased mobility due to worsening back pain. However, the later in life the diagnosis, the higher the chance for debilitating mobility issues over time.
In order for a doctor to diagnose SD, a person must undergo a battery of tests, some of which may include:
- X-rays
- Computed tomography, or CT scan.
- Myelography (x-ray utilizing specialized dye).
- Magnetic resonance imaging or MRI (uses magnetic waves instead of x-rays to view tissue and bone).
Once the tests are read by the physician, a diagnosis of SD can include one or all of the following results:
In x-rays, healthy vertebrae appear rectangular (see drop down box of healthy spine and spine with SD). However, the vertebrae of people with SD are wedge-shaped. If three or more consecutive vertebrae are wedged 5 degrees or more, then SD may be confirmed (usually in the thoracic region of the spine). The apex, or peak, of the curvature.
The long ligament that connects the front of the vertebra, called the anterior longitudinal ligament (see Image 3), thickens and can cause more pressure on the spine and vertebral wedging.
There also may be vertebral end plate irregularities, including Schmorl’s Nodes (see Image 4). These nodes appear on x-rays when disc cartilage is absorbed by, or protrudes into, the vertebral end plates. Sometimes these nodes can be so severe that SD can be misdiagnosed as infections or tumors.
Scheuermann’s Disease differs from Scoliosis (see Image 5) in that a person with scoliosis has a sideways curve to their spine, often in an S or C shape. A patient with Scheuermann’s Disease has a curve from the front of the spine to the back, causing the aforementioned hump or “hunchback”
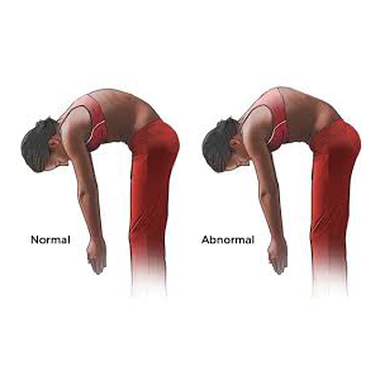
It is also important to note that the "Adam’s Forward Bend Test" for juvenile and adolescent scoliosis must be altered when assessing Scheuermann’s Disease. As the patient bends over, the tester must be behind the patient to identify the scoliosis (see Image 6), or side to side curve. For identifying SD, the tester must be BESIDE the patient (see Image 7) since the curvature is from front to back, or the accentuated curve may not be identified.
There is also a combination of Scheuermann’s Disease and Scoliosis called Kyphoscoliosis. This occurs when a person’s spine has both kyphosis (backwards) and lateral (side to side) curvature.
Juvenile Disc Disorder (Image 8) happens when adolescents develop early onset of degenerative disc disease. It is usually not associated with any spinal malalignment and typically occurs in the entire lumbar region of the spine.
There is also a combination of Scheuermann’s Disease and Scoliosis called Kyphoscoliosis. This occurs when a person’s spine has both kyphosis (backwards) and lateral (side to side) curvature.
Juvenile Disc Disorder (Image 8) happens when adolescents develop early onset of degenerative disc disease. It is usually not associated with any spinal malalignment and typically occurs in the entire lumbar region of the spine.
Causes
Scheuermann’s Disease is believed to be caused by an abnormality in vertebral bone growth, potentially by an interruption of blood flow to the vertebrae during adolescence (in periods of bone growth). As a result of these vascular abnormalities, the front (anterior) of the vertebrae grows faster than the back (posterior). This can cause the vertebral bodies to change from a healthy rectangular shape to triangular wedge shapes.
Other factors involved in this abnormal vertebral bone growth may include childhood osteoporosis and mechanical factors (heavy lifting, poor posture). Likely, there will be a combination of factors that comprise the root cause of the disease with mechanical factors only contributing to the severity of the disorder.
Other factors involved in this abnormal vertebral bone growth may include childhood osteoporosis and mechanical factors (heavy lifting, poor posture). Likely, there will be a combination of factors that comprise the root cause of the disease with mechanical factors only contributing to the severity of the disorder.
Effects
People diagnosed with SD tend to have certain physical characteristics that manifest as a result of the disease, or are seen in patients as precursors to a diagnosis. These bodily traits may include:
In addition, SD may be a predictor for adults developing severe thoracic and/or low back pain later in life. SD can result in a spinal degenerative process that causes significant interference in daily activities, due to pain and restriction of movement if left untreated. The disease may also cause ancillary problems involving the spine, including:
Spondylolithesis refers to the displacement of a vertebra in relation to the vertebrae below, and may be seen as a stress fracture in x-rays (usually affects the lumbar spine).
Spinal Stenosis is a narrowing of the spinal canal. This narrowing can cause pain and nerve irritation as spinal material closes around nerve roots and/or the spinal canal.
This stenosis can cause myelopathy, where a patient’s balance, muscle strength, and/or nerve reactivity may be permanently affected.
- Broad chests in men.
- Inability to sit or stand for any length of time due to pain.
- Elongated lungs can cause decreased lung capacity due to unusual chest cavity shape and the inability of the diaphragm to move adequately which causes a lack of breathing depth.
- Very tight lower back muscles and leg hamstrings.Growth spurts during adolescence are common.
- Fatigue
- Back pain, potentially in all spinal regions.
- Protrusion of buttocks, “athletic butt”.
In addition, SD may be a predictor for adults developing severe thoracic and/or low back pain later in life. SD can result in a spinal degenerative process that causes significant interference in daily activities, due to pain and restriction of movement if left untreated. The disease may also cause ancillary problems involving the spine, including:
Spondylolithesis refers to the displacement of a vertebra in relation to the vertebrae below, and may be seen as a stress fracture in x-rays (usually affects the lumbar spine).
Spinal Stenosis is a narrowing of the spinal canal. This narrowing can cause pain and nerve irritation as spinal material closes around nerve roots and/or the spinal canal.
This stenosis can cause myelopathy, where a patient’s balance, muscle strength, and/or nerve reactivity may be permanently affected.
Treatment
Treatment plans for patients diagnosed with SD depend on a number of factors, like patient age at the time of diagnosis, the degree of malalignment, and relative overall health.
If SD is confirmed during pre-pubescent or adolescent years (prior to the finalization of spinal formation), then physical therapy may be sufficient to correct a portion of the malalignment. Plans may include exercises to strengthen the muscles supporting the spine, stretching of hamstring and pectoral muscles, as well as limiting physical activities that involve constant pounding of the body.
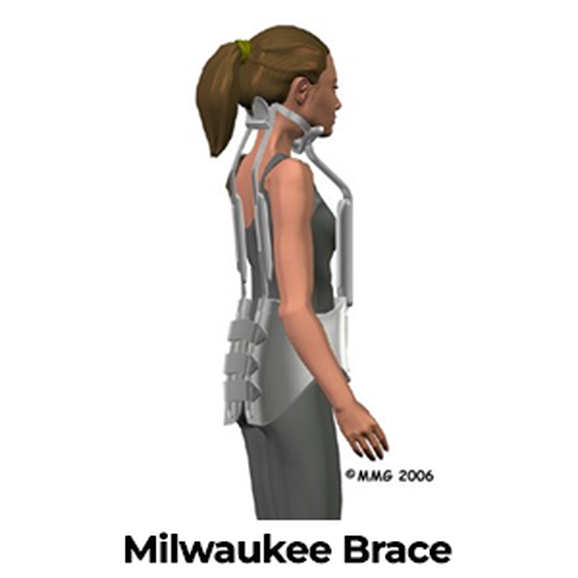
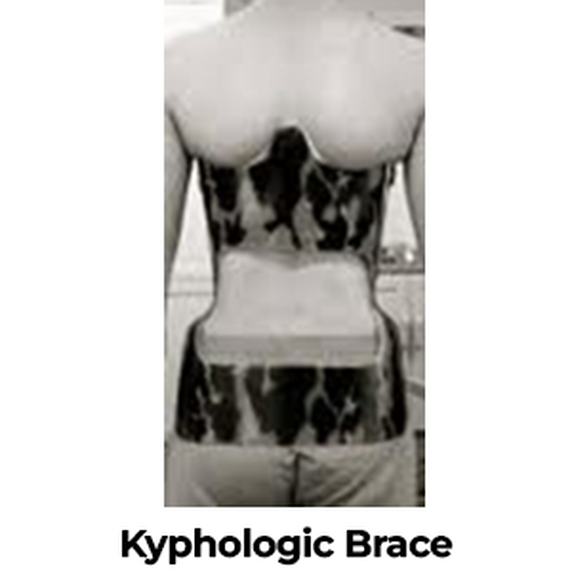
Braces that support the spine are an option (see Image 9) in situations where physical therapy is insufficient to correct a high percentage of the malalignments. Multiple studies have been published on the use of braces to help correct SD in pre-adult patients, and they vary in noting their effectiveness. There are primarily two types of braces used to help correct SD:
Remember, the effectiveness of any treatment, including physical therapy and bracing, depends on the level of malalignment and an individual’s specific circumstance.
Unfortunately, once a person’s spine forms (at about the age of 14 or 15), these bracing therapies will more than likely be ineffective.
- Physical Therapy
If SD is confirmed during pre-pubescent or adolescent years (prior to the finalization of spinal formation), then physical therapy may be sufficient to correct a portion of the malalignment. Plans may include exercises to strengthen the muscles supporting the spine, stretching of hamstring and pectoral muscles, as well as limiting physical activities that involve constant pounding of the body.
- Bracing
Braces that support the spine are an option (see Image 9) in situations where physical therapy is insufficient to correct a high percentage of the malalignments. Multiple studies have been published on the use of braces to help correct SD in pre-adult patients, and they vary in noting their effectiveness. There are primarily two types of braces used to help correct SD:
- Milwaukee Brace – consists of plastic molded to the patient’s specific waist, plus two bars in the back and one in the front. This brace is designed to help straighten the spine and keep an upright posture.
- The Milwaukee Brace is usually prescribed to be worn during waking hours but often times can be removed for bathing.
- Some studies note that there was marked improvement of curvature, ranging from 35% to 50% correction, following the use of the brace.
- On a side note, it is somewhat cumbersome and not cosmetically acceptable for many patients (think puberty and adolescence) so practical uses of the device vary by individual.
- Kyphologic Brace (Image 10) – Very similar in contour and shape to the Milwaukee Brace except with less material and is less cumbersome (also increases likelihood of prescribed use since it is also more cosmetically appealing).
- There are very limited case-studies and detailed reports on the long-term effectiveness of a Kyphologic Brace for treating Scheuermann’s Disease.
- Some short-term studies have shown that the average curvature correction varies, between 15% and 16.5%.
Remember, the effectiveness of any treatment, including physical therapy and bracing, depends on the level of malalignment and an individual’s specific circumstance.
Unfortunately, once a person’s spine forms (at about the age of 14 or 15), these bracing therapies will more than likely be ineffective.
Surgery
Young patients with Scheuermann’s Disease rarely require surgery to correct curvatures. However, older patients (whose spines have completed their growth cycle) who have their daily lives interrupted by pain and limited mobility may benefit from corrective spinal surgery.
Multiple surgical procedures exist that are designed to correct malalignments, improve function, and reduce back and limb pain. Some of these surgical options may include:
Each vertebra has two laminae, or bony appendages, that direct nerves to other parts of the body from the spinal cord. If these laminae become smaller, compression on the nerves result. This can cause pain, numbness, the sensation of “pins and needles”, or loss of movement. It can also be a painful surgery with long recovery periods.
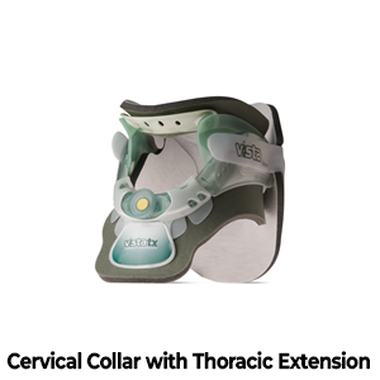
Cervical collar (See Image 11)
Cervical collar with thoracic extension (See Image 12)
Sacral/Lumbar Brace (see Image 13)
Multiple surgical procedures exist that are designed to correct malalignments, improve function, and reduce back and limb pain. Some of these surgical options may include:
- A spinal stenosis or foraminal laminectomy (is commonly referred to as a spinal “roto-rooter”) operation is designed to relieve the pressure on nerve roots or the spinal cord that is being compressed by discs or vertebrae.
Each vertebra has two laminae, or bony appendages, that direct nerves to other parts of the body from the spinal cord. If these laminae become smaller, compression on the nerves result. This can cause pain, numbness, the sensation of “pins and needles”, or loss of movement. It can also be a painful surgery with long recovery periods.
- Spinal fusion (also known as spondylodesis or spondylosyndesis) is used to join two or more unstable vertebrae. In some situations, Scheuermann’s Disease can cause vertebrae to become unstable and require surgery to solidify the spine.
- The fusion can involve one or all of the spinal regions; sacral, lumbar, thoracic, and cervical. It can be performed via the front (anterior), back (posterior), or both sides (combined) of the spine.
- A doctor (orthopedic spinal surgeon or neurosurgeon) will make the necessary incision and apply pressure in an attempt to straighten the curvature.
- Rods and screws are then inserted into the necessary vertebrae for support and strength.
- Bone tissue (from cadavers or grafts taken from the patient’s rib or pelvis) is then laid upon the spine. The bone can be ground and applied to fill gaps, or fragments can be tamped into place.
- Bone Morphogenic Protein (or BMP) may be used in lieu of, or in addition to, these bone grafts. BMP is a naturally occurring protein developed through gene research that aids in bone fusion. It can also be used in situations where a patient’s body is unable to fuse with cadaver bones or there is insufficient material to use from the patient’s own skeleton.
- The healing time from spinal fusion will vary by individual, but multiple studies have shown very good success rates in helping maintain or improve the quality of life for patients.
- Patients will be required to wear a brace following any type of spinal fusion. Below are examples of various types of spinal braces that I have worn:
Cervical collar (See Image 11)
Cervical collar with thoracic extension (See Image 12)
Sacral/Lumbar Brace (see Image 13)
Helpful tips
- Wash pads with shampoo and let dry for two days before wearing.
- Place the pads on an electric/gas dryer screen (used for shoes or sweaters) to help dry if necessary.
- Expect to get frustrated wearing the collar, they are tough to get accustomed to.
- Cut the tags off the back of shirts or wear tagless shirts when possible. This will help reduce itching.
Summary of Diagnosis and Treatments
The quality and quantity of long-term studies involving patients with Scheuermann’s Disease are quite disappointing. Some studies note that certain neurologists, neurosurgeons, and orthopedic spinal surgeons are seeing a higher rate of negative physical implications in older patients, including:
There is one point that remains worrisome in all studies:
The aforementioned physical and mental long-term difficulties associated with Scheuermann’s Disease are appearing in all types of patients, those medically treated and those who never sought medical help.
More detailed studies on the long-term effects of Scheuermann’s Disease are desperately needed. People afflicted with this disease (and their loved ones) need more accurate and timely information to properly address and prepare for life changing events.
- Acceleration of degenerative disc disease.
- Sedentary lifestyle as a result of radiating spinal pain which can affect the spinal cord.
- Multiple surgeries to correct malalignments.
- Debilitating lower back pain.
- Erosive spinal osteoarthritis.
- Significant mental stress associated with chronic pain.
- Depression and anxiety.
There is one point that remains worrisome in all studies:
The aforementioned physical and mental long-term difficulties associated with Scheuermann’s Disease are appearing in all types of patients, those medically treated and those who never sought medical help.
More detailed studies on the long-term effects of Scheuermann’s Disease are desperately needed. People afflicted with this disease (and their loved ones) need more accurate and timely information to properly address and prepare for life changing events.